Price transparency of prostate cancer care in the United States: An analysis of pricing and disclosure following the centers for medicare and medicaid mandate | Prostate Cancer and Prostatic Diseases
Abstract
Background
Starting January 1, 2021, Centers for Medicare and Medicaid Services required United States hospitals to publicly disclose prices of their services provided. We analyzed publicly-disclosed prices of prostate cancer-related services.
Methods
All United States hospitals were queried for publicly-disclosed prices of total and free prostate-specific antigen, prostate magnetic resonance imaging, prostate biopsy, radical prostatectomy, and intensity-modulated radiation therapy as of May 2022. Prices were adjusted by regional price parity. Hospitals disclosing prices were compared with non-disclosing hospitals.
Results
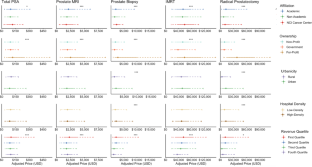
Of 6013 hospitals, 3840 (64%) disclosed pricing for at least one prostate cancer-related service. Compared to non-disclosing hospitals, disclosing hospitals had higher median gross annual revenue ($318,502,426 vs. $62,930,436, p < 0.001) and were more likely to be non-profit (56% vs. 30%, p < 0.001), academic-affiliated (46% vs. 13%, p < 0.001), and in neighborhoods with low hospital density (68% vs 62%, p < 0.001).
Self-pay prices were higher than insurance-negotiated prices for all services (p < 0.001) other than prostate biopsy.
The range of pricing was widest for self-pay prostatectomy, with a 32-fold difference from 90th to 10th percentile ($47,445 to $1476).
Self-pay prices of total prostate-specific antigen, magnetic resonance imaging, biopsy, intensity-modulated radiation therapy, and prostatectomy were higher at academic vs. non-academic, for-profit vs. non-profit hospitals, and hospitals in the top quartile of gross annual revenue vs. the third and fourth quartiles (p < 0.01).
Self-pay prices of prostate biopsy and prostatectomy were higher in urban vs. rural neighborhoods and neighborhoods with high vs. low hospital density (p < 0.001).
Conclusions
Self-pay prices of prostate cancer services were generally higher than insurance-negotiated prices and were higher at for-profit hospitals, academic hospitals, and hospitals in the highest quartile of gross annual revenue.
Higher neighborhood hospital density was not associated with higher likelihood of price disclosure nor lower pricing of services, suggesting that local competition does not lead to lower prices and may disincentivize disclosure of prices.
This is a preview of subscription content, access via your institution
Access options
Subscribe to Journal
Get full journal access for 1 year
$119.00
only $29.75 per issue
All prices are NET prices.
VAT will be added later in the checkout.
Tax calculation will be finalised during checkout.
Buy article
Get time limited or full article access on ReadCube.
$32.00
All prices are NET prices.
Data availability
The data used in this study were obtained under license from Turquoise Health. Researchers interested in these data may visit https://turquoise.health for additional information on acquiring this dataset.
References
Medicare and Medicaid Programs: CY 2020 Hospital Outpatient PPS Policy Changes and Payment Rates and Ambulatory Surgical Center Payment System Policy Changes and Payment Rates. Price Transparency Requirements for Hospitals To Make Standard Charges Public. 84 Fed. Reg. 65524-65606 (November 27, 2019)
Xiao R, Rathi VK, Gross CP, Ross JS, Sethi RKV. Payer-Negotiated Prices in the Diagnosis and Management of Thyroid Cancer in 2021 [published online ahead of print, 2021 Jun 4]. JAMA. 2021;326:184–5. https://doi.org/10.1001/jama.2021.8535
American Cancer Society. Cancer Facts & Figures 2021. Atlanta: American Cancer Society; 2021.
Mahal BA, Aizer AA, Ziehr DR, Hyatt AS, Lago-Hernandez C, Chen Y-W, et al. The association between insurance status and prostate cancer outcomes: implications for the Affordable Care Act. Prostate Cancer Prostatic Dis. 2014;17:273–9.
Agarwal A, Dayal A, Kircher SM, Chen RC, Royce TJ. Analysis of price transparency via national cancer institute-designated cancer centers’ Chargemasters for prostate cancer radiation therapy [published correction appears in JAMA Oncol. 2020 Mar 1;6(3):444]. JAMA Oncol. 2020;6:409–12.
Anderson GF. From ‘soak the rich’ to ‘soak the poor’: recent trends in hospital pricing. Health Aff (Millwood). 2007;26:780–9.
“Press Release CMS Proposes Rule to Increase Price Transparency, Access to Care, Safety & Health Equity.” Centers for Medicare and Medicaid Services, https://www.cms.gov/newsroom/press-releases/cms-proposes-rule-increase-price-transparency-access-care-safety-health-equity.
“Revenue Trends at U.S. Hospitals.” Definitive Healthcare, https://www.definitivehc.com/blog/revenue-trends-at-u.s.-hospitals.
Lu AJ, Chen EM, Vutam E, Brandt J, Sadda P. Price transparency implementation: Accessibility of hospital chargemasters and variation in hospital pricing after CMS mandate. Health (Amst) 2020;8:100443.
Hut, Nick. “CMS Finalizes Changes to the Price Transparency Penalty, Inpatient-Only List and More for 2022.” Healthcare Financial Management Association, https://www.hfma.org/topics/news/2021/11/cms-finalizes-changes-to-the-price-transparency-penalty--ipo-lis.html.
Acknowledgements
Jonathan Shoag is supported by the Frederick J. and Theresa Dow Fund of the New York Community Trust, the Vinney Scholars Award, and a Damon Runyon Cancer Research Foundation Physician Scientist Training Award. The work presented here was not directly funded by an outside organization or sponsor. Jonathan Shoag had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brant, A., Lewicki, P., Rhodes, S. et al. Price transparency of prostate cancer care in the United States: An analysis of pricing and disclosure following the centers for medicare and medicaid mandate. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00643-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00643-9
Subjects

Comments
Post a Comment