How numbers help patients more than vague terms
How numbers help patients more than vague terms
Speaking Your Language: Why Numbers Matter More Than Words in Prostate Cancer Decisions
A Guide for the Informed Prostate Cancer Patient
IPCSG Newsletter Special Report - October 2025
The Problem: When "Common" and "Rare" Mean Different Things
As engineers, some of us are comfortable with numbers. We understand that precision matters—that 0.005 tolerance isn't the same as 0.05. But when it comes to our health, doctors often speak to us in vague terms like "rare," "common," or "unlikely." These words mean different things to different people, and that ambiguity can lead to poor decisions about our prostate cancer care.
A groundbreaking paper published in the Journal of the American Medical Association (JAMA) in September 2025 confirms what many of us have suspected: clear numbers help patients make better decisions than vague verbal descriptions.
Dr. Angela Fagerlin of the University of Utah, one of the study's authors, explains the stakes: "In breast cancer or prostate cancer, patients will say, 'The most important thing to me is to increase my likelihood of survival.' But then they're making decisions that are actually decreasing their likelihood of survival...because they didn't understand the numbers."
Why This Matters for Prostate Cancer Patients
For men facing prostate cancer decisions, the choices are often complex and deeply personal:
- Active surveillance vs. immediate treatment: What's your actual risk of progression?
- Surgery vs. radiation: What are the real differences in side effect rates?
- Treatment trade-offs: How much does a treatment reduce your cancer risk versus increasing erectile dysfunction or incontinence?
The 2024 Advanced Prostate Cancer Consensus Conference emphasized that treatment decisions should be individualized based on patient and cancer characteristics. But you can't make an informed choice if the information isn't clear.
The "There's a Chance" Problem
This is particularly troubling when discussing side effects. A groundbreaking 2024 study published in Prostate Cancer and Prostatic Diseases analyzed 50 actual prostate cancer treatment consultations and found shocking variation in how doctors communicate critical side effects:
For Erectile Dysfunction After Surgery:
- 15% of consultations: Never mentioned it at all
- 47% of consultations: Either just named it or used vague terms like "some risk"
- Only 30% of consultations: Actually gave numbers with a timeline
For Urinary Incontinence After Radiation:
- 22% of consultations: Never mentioned irritative urinary symptoms
- 42% of consultations: Never mentioned erectile dysfunction risks
- Only 3-8% of consultations: Quantified side effects with timelines
The study found that when doctors did mention side effects, they often used phrases like "patients do well after surgery, with minimal effect on potency" or "there's a chance of some issues." These statements provide no actionable information for decision-making.
Recent data shows these decisions matter enormously. The 2025 NCCN Guidelines report that approximately 299,010 new prostate cancer cases will be diagnosed in the United States in 2024. With a 5-year relative survival rate of 97% for all stages combined, many men face the challenge of choosing between treatment options with different benefit-risk profiles.
The Five Key Principles of Clear Medical Communication
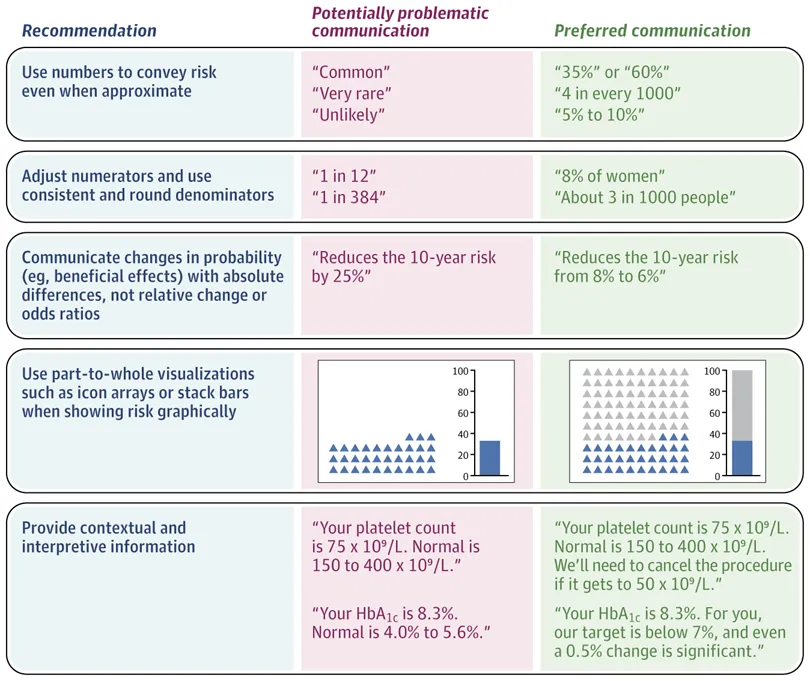
The JAMA paper outlines five evidence-based strategies that doctors should use when communicating with patients:
1. Use Numbers, Not Vague Words
Bad: "The risk of this side effect is rare."
Good: "4 out of 1,000 men experience this side effect."
Why? A 1% risk may sound low when discussing a fever after a flu vaccine, but a 1% risk of incontinence after prostate surgery may feel very different to you.
2. Use Consistent Denominators
Bad: "The risk is 1 in 112 with Treatment A versus 1 in 384 with Treatment B."
Good: "The risk is 8.9 per 1,000 with Treatment A versus 2.6 per 1,000 with Treatment B."
Research shows that more patients correctly identify which treatment is safer when consistent denominators are used.
3. Present Absolute Risk, Not Just Relative Risk
Bad: "This treatment reduces your 10-year cancer death risk by 25%."
Good: "This treatment reduces your 10-year cancer death risk from 8% to 6%."
The first statement sounds impressive, but the second shows you the actual impact on your life. A 25% relative reduction could mean reducing risk from 8% to 6%, or from 0.004% to 0.003%—vastly different real-world impacts.
4. Use Visual Aids
Icon arrays and bar charts help make numbers concrete. For example, showing 100 human figures with 8 highlighted (representing the 8% baseline risk) and then 6 highlighted (representing the 6% risk after treatment) makes the benefit immediately clear.
5. Provide Context for Unfamiliar Numbers
As engineers, we appreciate comparable benchmarks. Medical radiation exposure provides a perfect example of this principle in action.
Making Sense of Radiation Risk: An Engineering Approach
One area where comparable risk communication particularly helps is understanding radiation exposure from imaging tests. Many prostate cancer patients undergo CT scans, bone scans, and other imaging that involves ionizing radiation.
Here's how medical professionals can make these numbers meaningful:
Natural Background Radiation
- Average annual exposure: 3 mSv (millisieverts)
- Living in Colorado or New Mexico adds: 1.5 mSv per year due to altitude
- Daily natural background: approximately 0.008 mSv
Air Travel as a Benchmark
- Coast-to-coast round-trip flight: 0.03 mSv
- 10-hour airline flight: 0.03 mSv
- Transatlantic flight (e.g., New York to London): 0.01 mSv
Common Medical Imaging
- Single chest X-ray: 0.1 mSv (equivalent to about 10 days of natural background radiation, or 3 coast-to-coast flights)
- Mammogram: 0.4-0.6 mSv (equivalent to 12-20 transcontinental flights)
- CT scan of abdomen and pelvis: 10 mSv (equivalent to about 3 years of background radiation, or 300-400 transcontinental flights)
- Full-body CT scan: 10 mSv
- Bone scan (common in prostate cancer staging): 3-7 mSv
Putting It in Perspective Dr. Rebecca Smith-Bindman of UC San Francisco notes: "It's often said that the radiation dose of a chest X-ray is comparable to flying across the continent. But a CT scan can be comparable to 500 transcontinental flights."
For context, radiation workers are limited to 50 mSv per year, and research suggests that below 100 mSv from all sources combined, risks are either too small to observe or nonexistent. To put this in perspective, astronauts can be exposed to over 150 mSv annually.
Current Prostate Cancer Screening and Imaging Recommendations
The landscape of prostate cancer detection has evolved significantly:
2023 AUA/SUO Guidelines for Early Detection
- PSA remains the first-line screening test
- Begin screening at age 45-50 for average-risk men
- Begin at age 40-45 for high-risk men (Black ancestry, germline mutations, strong family history)
- Screen every 2-4 years for men aged 50-69
- MRI may be used prior to initial biopsy to increase detection of Grade Group 2+ cancer
Breakthrough Research: The Gothenburg-2 Trial Published in the New England Journal of Medicine (2022, updated 2024), this trial demonstrated that using MRI before biopsy significantly reduced diagnosis of clinically insignificant cancers. Key findings:
- MRI-targeted biopsy approach eliminated more than half of clinically insignificant cancer diagnoses
- The relative risk of detecting clinically insignificant cancer was 0.43 with MRI-targeted biopsy compared to systematic biopsy
- Risk of missing aggressive cancer was very low
- At repeat screening rounds, the benefit was even greater (relative risk 0.25)
This research suggests that modern screening protocols using PSA, MRI, and targeted biopsies can reduce overdiagnosis while maintaining detection of dangerous cancers.
What This Means for Treatment Decisions
Understanding side effect rates with precise numbers becomes critical when weighing treatment options. But first, you need to know just how wide the variation in outcomes can be—and why asking for YOUR specific numbers matters.
The Real Numbers (Not "There's a Chance")
A comprehensive 2022 SEER-Medicare study analyzing 67,527 patients provides actual population-level data:
Radical Prostatectomy (Surgery) - Single Treatment
- Erectile dysfunction diagnosis: 56.1% (more than 1 in 2 men)
- Urinary incontinence diagnosis: 44.5% (nearly 1 in 2 men)
- Long-term incontinence requiring pads: approximately 20% (1 in 5 men)
- Urethral stricture: 5.35% (about 1 in 19 men)
- Cystitis: 20.3% (about 1 in 5 men)
Radiation Therapy (RT) - Single Treatment
- Erectile dysfunction diagnosis: 30.4% (about 3 in 10 men)
- Urinary incontinence diagnosis: 29.7% (about 3 in 10 men)
- Long-term erectile dysfunction: over 50% by some measures
- Urethral stricture: 8.44% (about 1 in 12 men)
- Cystitis: 33.1% (1 in 3 men)
- Proctitis (bowel inflammation): 14.7% (about 1 in 7 men)
- Long-term bothersome bowel symptoms: up to 17% (about 1 in 6 men)
Combined Treatments (Multi-Modal Therapy) If you need both surgery AND radiation:
- Incontinence medication use: 12.0% (vs. 9.8% for RT-only, 8.3% for RP-only)
- Overall incontinence therapy needed: 18.5% (nearly 1 in 5 men)
- Radiation followed by surgery has the worst functional outcomes of all approaches
Other Side Effects Often Not Discussed
- Up to 70% of men experience sex-related incontinence (leaking during orgasm) after treatment
- Nearly 80% reduction in ejaculate volume after radiation (prostate produces most of the fluid)
- For brachytherapy specifically: ED in 14-35% (much lower than other treatments)
But These Are AVERAGES—Your Numbers May Be Different
Here's where "there's a chance" becomes particularly deceptive. Your actual risk depends on:
- Your age: Younger men typically recover function better
- Your baseline function: If you have excellent erectile function before treatment, your odds of recovery are better
- Nerve-sparing technique: Can dramatically reduce ED risk in surgery
- Surgeon/radiation oncologist experience: High-volume centers often have better outcomes
- Treatment combinations: Multi-modal therapy significantly worsens outcomes
A precision estimate might sound like: "You're 52, your baseline erectile function is excellent, and I use nerve-sparing technique. Your likelihood of regaining baseline function within a year is upwards of 80%" versus just "there's a chance of erectile dysfunction."
Active Surveillance Recent 10-year data from the UK ProtecT trial shows:
- 99% survival rate across all groups (surgery, radiation, active surveillance)
- 54.8% of men on active surveillance eventually received treatment
- Metastatic cancer risk: 6.0% with surveillance vs. 2.3% with surgery vs. 2.7% with radiation
- About 45% of men on active surveillance avoided treatment and its side effects entirely while maintaining excellent outcomes
These numbers help frame the real trade-offs you're making, not just abstract risks.
New Treatment Advances in 2024-2025
The Advanced Prostate Cancer Newsletter from ZERO Prostate Cancer highlights several breakthrough developments:
For Metastatic Castration-Resistant Prostate Cancer (mCRPC)
- Pluvicto (177-Lutetium PSMA-617) showing promise before chemotherapy
- New radioligand therapy (177-Lutetium PNT2002) in trials
- Combination therapies expanding: talazoparib with enzalutamide now approved for patients with mutations beyond BRCA
These advances emphasize the growing importance of genetic testing for personalized treatment decisions.
How to Apply This Information
The research is clear, but only 34% of US adults can perform simple numerical tasks like identifying the largest value in a list. Here's how you can advocate for clearer communication:
Questions to Ask Your Doctor
- "Can you give me the actual numbers?"
Don't accept "rare," "common," or "there's a chance"—ask for "X out of 100 men" or percentages. - "What are MY specific numbers based on my age, baseline function, and your experience?"
Don't settle for population averages. Studies show outcomes vary dramatically based on individual factors. - "What's the absolute difference?"
If a treatment "reduces risk by 30%," ask what your actual risk goes from and to. - "What percentage of YOUR patients experience each side effect?"
High-volume, experienced surgeons and radiation oncologists often have better outcomes than population averages. - "When do these side effects occur and how long do they last?"
"50% experience erectile dysfunction" is useless without knowing: at what timepoint? Is this temporary or permanent? Does function improve over 2 years? - "How does this compare to something I understand?"
For radiation: "How many cross-country flights is this equivalent to?"
For side effects: "Out of 100 men like me, how many experience this?" - "Can you show me this visually?"
Ask for charts or diagrams, or use tools like iconarray.com yourself. - "What's my baseline risk without treatment?"
You can't evaluate a treatment benefit without knowing your starting point. - "If I need combination therapy later, how much do the side effect risks increase?"
Multi-modal therapy has significantly worse outcomes than single treatment—you need these numbers upfront.
Resources and Tools
Several organizations provide excellent fact-box tools for understanding treatment trade-offs:
- Harding Center for Risk Literacy (Max Planck Institute): Provides visual fact boxes for medical decisions
- NCCN Guidelines for Patients: Free, evidence-based guides in plain language
- PCRI Staging Guide: Color-coded system (Sky, Teal, Azure, Indigo, Royal) that simplifies complex staging
- ZERO Prostate Cancer: Comprehensive resources for patients and caregivers
The Bottom Line
As Dr. Fagerlin's research shows, understanding the numbers empowers you to make decisions that truly align with your values and priorities. Whether you're an engineer comfortable with technical data or someone who prefers visual aids, you have the right to clear, numerical information about your prostate cancer care.
The goal isn't to turn every patient into a statistician—it's to ensure that when you say, "The most important thing to me is to avoid incontinence," you choose the treatment that actually gives you the best chance of achieving that goal.
Don't settle for vague terms. Ask for numbers. Demand clarity. Your prostate cancer decisions are too important for anything less.
References and Sources
- Zikmund-Fisher BJ, Thorpe A, Fagerlin A. How to Communicate Medical Numbers. JAMA. 2025 Sep 24. doi:10.1001/jama.2025.13655. Available at: https://jamanetwork.com/journals/jama/article-abstract/2839303
- Schwitzer G. How numbers help patients more than vague terms. Gary Schwitzer's HealthNewsReview Substack. 2025. Available at: https://garyschwitzer.substack.com
- Ahmed HU, El-Shater Bosaily A, Brown LC, et al. Communicating study results to our patients: Which way is best? Indian Journal of Orthopaedics. 2008;42(2):140-143. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2759623/
- Edwards A, Elwyn G, Mulley A. Communicating risk to patients and the public. British Journal of General Practice. 2012;62(597):213-216. Available at: https://bjgp.org/content/62/597/213
- van Stam MA, Aaronson NK, Bosch JLHR, et al. Variation in communication of side effects in prostate cancer treatment consultations. Prostate Cancer and Prostatic Diseases. 2024;27:178-185. doi:10.1038/s41391-024-00806-2. Available at: https://www.nature.com/articles/s41391-024-00806-2
- Resnick MJ, Barocas DA, Morgans AK, et al. Functional outcomes after prostate cancer treatment: A comparison between single and multiple modalities. Urologic Oncology: Seminars and Original Investigations. 2023;41(2):97.e13-97.e20. doi:10.1016/j.urolonc.2022.09.018. Available at: https://www.sciencedirect.com/science/article/abs/pii/S1078143922002745
- American Cancer Society. Understanding Radiation Risk from Imaging Tests. Available at: https://www.cancer.org/cancer/diagnosis-staging/tests/imaging-tests/understanding-radiation-risk-from-imaging-tests.html
- Radiological Society of North America. Radiation Dose from X-Ray and CT Exams. Available at: https://www.radiologyinfo.org/en/info/safety-xray
- Centers for Disease Control and Prevention. Facts About Radiation from Air Travel. Updated February 20, 2024. Available at: https://www.cdc.gov/radiation-health/data-research/facts-stats/air-travel.html
- Smith-Bindman R. Radiation From CT Scans May Raise Cancer Risk. NPR Health. December 15, 2009. Available at: https://www.npr.org/2009/12/15/121436092/radiation-from-ct-scans-may-raise-cancer-risk
- Hugosson J, Månsson M, Wallström J, et al. Prostate Cancer Screening with PSA and MRI Followed by Targeted Biopsy Only. New England Journal of Medicine. 2022;387(23):2126-2137. doi:10.1056/NEJMoa2209454. Available at: https://www.nejm.org/doi/full/10.1056/NEJMoa2209454
- Hugosson J, Godtman RA, Wallstrom J, et al. Results after Four Years of Screening for Prostate Cancer with PSA and MRI. New England Journal of Medicine. 2024;391(12):1083-1095. doi:10.1056/NEJMoa2406050. Available at: https://www.nejm.org/doi/abs/10.1056/NEJMoa2406050
- Eastham JA, Auffenberg GB, Barocas DA, et al. EAU-EANM-ESTRO-ESUR-ISUP-SIOG Guidelines on Prostate Cancer. Part II-2024 Update: Treatment of Relapsing and Metastatic Prostate Cancer. European Urology. 2024;86(2):164-182. doi:10.1016/j.eururo.2024.04.010. Available at: https://pubmed.ncbi.nlm.nih.gov/38688773/
- Gillessen S, Bossi A, Davis ID, et al. Management of Patients with Advanced Prostate Cancer. Report from the 2024 Advanced Prostate Cancer Consensus Conference (APCCC). European Urology. 2025;87(2):157-216. doi:10.1016/j.eururo.2024.09.017. Available at: https://www.sciencedirect.com/science/article/pii/S0302283824026101
- National Comprehensive Cancer Network. NCCN Guidelines for Patients: Early-Stage Prostate Cancer, 2025. Available at: https://www.nccn.org/patients/guidelines/content/PDF/prostate-early-patient.pdf
- National Comprehensive Cancer Network. NCCN Guidelines for Patients: Advanced-Stage Prostate Cancer, 2025. Available at: https://www.nccn.org/patients/guidelines/content/pdf/prostate-advanced-patient.pdf
- Carroll PH, Mohler JL. NCCN Guidelines® Insights: Prostate Cancer, Version 3.2024. Journal of the National Comprehensive Cancer Network. 2024;22(3):140-150. doi:10.6004/jnccn.2024.0019. Available at: https://jnccn.org/view/journals/jnccn/22/3/article-p140.xml
- Wei JT, Barocas D, Carlsson S, et al. Early Detection of Prostate Cancer: AUA/SUO Guideline (2023). American Urological Association. Available at: https://www.auanet.org/guidelines-and-quality/guidelines/early-detection-of-prostate-cancer-guidelines
- ZERO Prostate Cancer. Winter 2024/2025 Advanced Prostate Cancer Newsletter. Available at: https://zerocancer.org/newsletters/advanced-prostate-cancer/2024-2025
- Prostate Cancer Research Institute. 2025 Midyear Update. Available at: https://pcri.org/2025-midyear-update
- U.S. Preventive Services Task Force. Prostate Cancer: Screening. May 8, 2018. Available at: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/prostate-cancer-screening
- Centers for Disease Control and Prevention. Should I Get Screened for Prostate Cancer? Updated February 11, 2025. Available at: https://www.cdc.gov/prostate-cancer/screening/get-screened.html
This article is provided for educational purposes as part of the Informed Prostate Cancer Support Group newsletter. It is not intended to replace professional medical advice. Always consult with your healthcare team about your specific situation.


Comments
Post a Comment