The AI Revolution in Cancer Care: Separating Promise from Reality
The Unseen Revolution: How Artificial Intelligence Is Redefining Cancer Care | NEJM AI Sponsored
This paper is sponsored content provided by Viz.ai. It has not been peer-reviewed or endorsed by NEJM AI and does not reflect the perspectives of the journal or its editors. Learn more about sponsored content and our business model here.
BLUF (Bottom Line Up Front)
Artificial intelligence is rapidly transforming cancer care through improved diagnostic accuracy, personalized treatment planning, and early detection capabilities. As of December 2025, the FDA has authorized approximately 950 AI-enabled medical devices, with significant recent approvals for cancer care including ArteraAI Prostate (first AI tool authorized to prognosticate long-term outcomes in prostate cancer) and Clairity Breast (first AI platform to predict five-year breast cancer risk from mammograms alone). While AI shows genuine promise in improving screening accuracy, predicting treatment responses, and enabling earlier detection through liquid biopsies and advanced imaging analysis, significant challenges remain including algorithmic bias, limited diverse training datasets, high implementation costs, and regulatory gaps. For prostate cancer patients, AI-powered tools are now commercially available for risk stratification, predicting hormone therapy benefit, and improving biopsy accuracy. However, current AI applications are best viewed as augmentation tools that support—rather than replace—physician judgment, and their effectiveness varies significantly across different patient populations.
Fact-Check of the Submitted Article
The article submitted for review makes several accurate claims but also includes some overstated promises and unsubstantiated assertions:
Accurate Claims:
- AI can detect early signs of toxicity and disease progression
- Multiple data streams (genomics, imaging, wearables, patient-reported outcomes) can be integrated
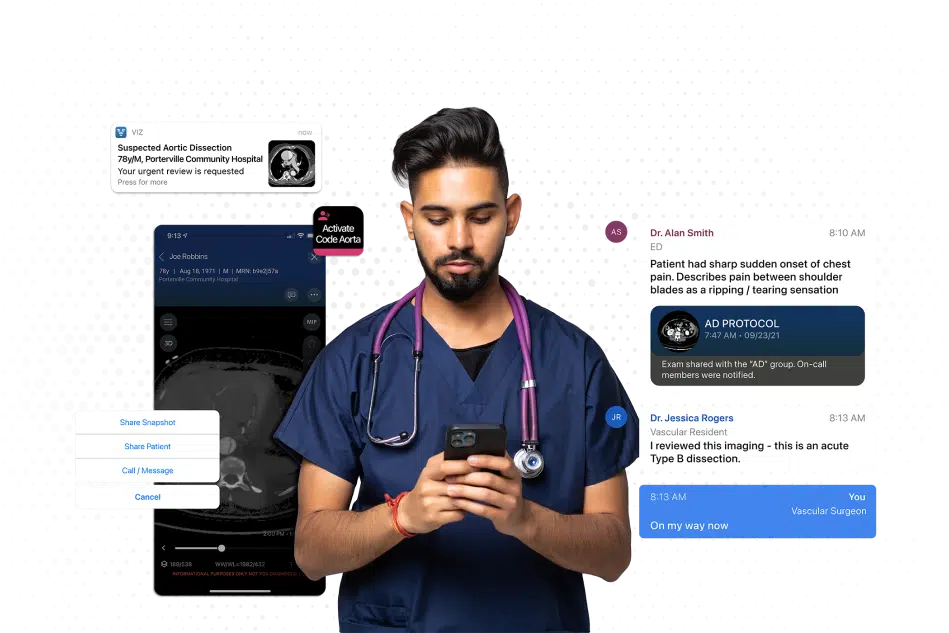
- Emergency medicine has demonstrated successful AI implementation for stroke detection
- Algorithmic bias and data quality issues are significant concerns
- Cultural and organizational barriers exist in healthcare AI adoption
Overstated or Unsubstantiated Claims:
- "Continuous monitoring" and "real-time care" described in the article remains largely aspirational rather than currently deployed in routine practice
- The claim that AI could predict neutropenic fever "days before fever develops" lacks specific clinical validation evidence
- The economic savings calculations appear speculative without cited supporting studies
- The article is sponsored content from Viz.ai (a stroke detection AI company) but discusses cancer care broadly, creating potential conflicts of interest
Missing Context:
- The article underemphasizes current limitations and validation gaps
- Limited discussion of the significant disparity in AI access between academic centers and community practices
- Insufficient attention to racial and ethnic bias in current AI systems
The Reality of AI in Cancer Care Today
Diagnostic Applications: From Promising to Proven
AI has made its most significant validated impact in cancer imaging and pathology. In breast cancer screening, the Swedish MASAI clinical trial reported in 2024 that AI-assisted workflows reduced radiologist workload by 44% while maintaining comparable clinical performance metrics. AI systems now match or exceed expert radiologists in detecting breast cancer on mammograms, with some tools achieving 94% sensitivity for early-stage disease detection.
For prostate cancer specifically, the FDA granted de novo authorization to ArteraAI Prostate in August 2025, marking it as the first AI-powered tool authorized to prognosticate long-term outcomes in patients with localized disease. This multimodal AI system analyzes digital pathology images plus clinical data to predict 10-year risk of distant metastasis and prostate cancer-specific mortality. In validation studies using data from multiple phase 3 trials, the ArteraAI test demonstrated 9.2% to 14.6% relative improvement over National Comprehensive Cancer Network risk stratification models across all endpoints at median follow-up of 11.4 years.
Similarly significant, the FDA granted de novo authorization to Clairity Breast in June 2025—the first AI platform that predicts a woman's five-year breast cancer risk using only a standard mammogram, without requiring family history or questionnaire data.
In pathology, AI tools like Paige Prostate Detect (which received FDA approval in March 2024 for second review of prostate cancer diagnosed using core needle biopsies) have shown improved detection rates for clinically significant prostate cancer. Multiple studies demonstrate that AI assistance helps pathologists identify micrometastases and rare cancer subtypes that might otherwise be overlooked, with particular benefits for less experienced pathologists or challenging cases.
Liquid Biopsy and Early Detection: The Next Frontier
One of the most exciting developments involves AI-enhanced liquid biopsy technologies. In June 2024, researchers at Weill Cornell Medicine reported development of an ultrasensitive liquid biopsy method powered by AI that showed unprecedented sensitivity in predicting cancer recurrence by detecting tumor DNA in blood samples. The technology uses whole-genome sequencing of DNA in blood samples, gathering much more "signal" than previous approaches that targeted relatively small sets of cancer-associated mutations.
The Orion AI model, developed in 2024, analyzes circulating orphan non-coding RNAs (oncRNAs) for early detection of non-small cell lung cancer. In a study of 1,050 treatment-naïve individuals (419 lung cancer patients and 631 matched controls), Orion achieved an area under the curve (AUC) of 0.97 with 94% sensitivity at 90% specificity in cross-validation. The DELFI model for evaluating cell-free DNA fragmentation achieved 94% sensitivity and 80% specificity for early-stage lung cancer while reducing false-positive rates by 50% compared to standard low-dose CT scanning.
A comprehensive review published in December 2024 examined exosome-based diagnostics, finding that these tiny cellular messengers carry molecular signatures of cancerous cells and can be collected from blood or urine. AI systems scanning vast molecular datasets are accelerating the identification of reliable cancer biomarkers from these exosomes, potentially enabling routine non-invasive cancer tracking.
Treatment Personalization: Matching Patients to Therapies
AI's ability to predict which patients will benefit from specific treatments represents perhaps its most clinically actionable application. For prostate cancer patients, this is particularly relevant. Data presented at the 2025 American Society of Clinical Oncology Annual Meeting showed that the ArteraAI multimodal AI algorithm could accurately identify which patients with high-risk non-metastatic prostate cancer were most likely to benefit from adding abiraterone acetate plus prednisone ± enzalutamide to standard androgen deprivation therapy in the STAMPEDE trial. The tool identified 34% of patients who may benefit from short-term hormone therapy, while also identifying patients who could safely avoid hormone therapy and its significant side effects.
Stanford Medicine researchers reported in January 2025 development of MUSK (Multimodal Understanding of disease using unpaired data from medical images and clinical text), an AI foundation model that combines data from medical images with text to predict cancer prognoses and treatment responses. Unlike previous approaches requiring carefully paired data, MUSK can use unpaired multimodal data, making it more practical for real-world implementation.
In radiation oncology, AI-assisted treatment planning has reduced the time required to design complex treatments while improving plan quality and consistency. Multiple studies published in 2024-2025 demonstrate fully automated machine-learning-based workflows for radiation treatment planning in prostate cancer, with some systems achieving treatment plans comparable to those created by experienced dosimetrists in a fraction of the time.
The Reality of "Continuous Monitoring"
While the submitted article envisions comprehensive continuous monitoring through wearables and multiple data streams, this remains largely aspirational in current clinical practice. Most AI applications in cancer care remain episodic rather than continuous. The integration of wearable device data, liquid biopsies, patient-reported outcomes, and laboratory studies into unified AI-driven monitoring systems exists primarily in research settings and select academic medical centers rather than routine care.
A 2025 review of digital sensing technologies in cancer care noted that while portable and point-of-care diagnostic tools are improving accessibility and enabling rapid decision-making, the integration of these technologies into continuous monitoring workflows faces significant barriers including data fragmentation, interoperability challenges, and reimbursement uncertainties.
The Prostate Cancer Patient Perspective
For IPCSG members and prostate cancer patients generally, several AI applications are now clinically available or emerging:
Currently Available:
-
ArteraAI Prostate Test: Commercial availability with Medicare Part B coverage (zero out-of-pocket cost for Medicare patients). Provides risk stratification for localized prostate cancer and prediction of hormone therapy benefit. Results available within 1-2 days after receipt of specimen.
-
Paige Prostate Detect: FDA-approved AI assistance for pathology review of prostate biopsies, helping ensure accurate detection and grading.
-
AI-Enhanced MRI Analysis: Multiple AI tools now assist radiologists in identifying suspicious lesions on prostate MRI, improving detection accuracy and reducing interpretation time. A 2025 study in JAMA Network Open found that AI-assisted identification of prostate cancer in magnetic resonance images improved detection rates compared to unassisted review.
Emerging Applications:
-
PATHOMIQ_PRAD: Licensed exclusively by Myriad Genetics in February 2025 for prostate cancer prognosis in the US. Uses AI to decode hidden information from morphological structures in pathology images to predict outcomes, treatment responses, and genotype mutations.
-
Liquid Biopsy for Prostate Cancer Monitoring: Multiple platforms in development using AI to analyze circulating tumor DNA for minimal residual disease detection and treatment response monitoring.
-
Radiotherapy Optimization: AI systems that automatically generate and optimize radiation treatment plans, potentially reducing treatment planning time and improving consistency.
The Critical Challenges
Algorithmic Bias and Health Equity
One of the most significant concerns about AI in cancer care involves algorithmic bias. Research consistently demonstrates that AI/ML models trained on homogeneous datasets often fail to account for the needs of historically marginalized populations, leading to disparities in diagnostic accuracy and treatment recommendations.
A study examining FOXA1 and TP53 mutations in prostate cancer found significant frequency differences between Black and white men, yet most AI models are trained on predominantly white patient populations. If AI models are trained on biased or incomplete data that overlooks certain racial, ethnic, or socioeconomic groups, they risk reinforcing and deepening existing inequalities in cancer care.
A 2024 JMIR Cancer article noted that without incorporating data from underrepresented groups, AI systems risk perpetuating existing healthcare disparities. In dermatology AI applications, for example, several studies examining cancer detection algorithms were found to include predominantly white populations or did not specify the racial and ethnic makeup of training populations, potentially leading to reduced accuracy in patients with darker skin tones.
Multiple reviews published in 2024-2025 emphasize that achieving equitable AI integration requires diverse and representative datasets, robust bias detection and correction methods, enhanced transparency and explainability, and inclusive development practices involving ethicists, sociologists, and representatives from marginalized communities.
Data Quality and Integration
Healthcare data remain fragmented across incompatible systems. Electronic health records designed for billing rather than clinical intelligence store information in formats that resist integration and analysis. Laboratory systems, imaging archives, and pharmacy databases operate in isolation, creating data silos that mirror the fragmentation of healthcare delivery itself.
Even when data can be integrated, quality issues abound. Missing values, inconsistent coding, and variable data collection practices create the "garbage in, garbage out" problem that undermines AI performance. A systematic review of FDA-cleared AI/ML devices found that standardized efficacy, safety, and risk assessment reporting remains inadequate, underscoring the need for dedicated regulatory pathways and robust postmarket surveillance.
Regulatory Evolution
As of July 2024, the FDA reports approximately 950 FDA-cleared AI/ML-enabled medical devices, with roughly 100 new approvals annually. However, the regulatory framework continues to evolve to accommodate AI technologies that learn and adapt over time.
In December 2024, the FDA issued finalized recommendations to streamline approval of AI/ML devices, recognizing the need for more flexible review processes and proposing "Predetermined Change Control Plans" that allow developers to update AI software (for example, to support additional scanners or adapt to new data sources) without restarting lengthy approval processes.
However, significant gaps remain. Most FDA-cleared AI products have been evaluated through 510(k) clearance (demonstrating substantial equivalence to existing devices) rather than through more rigorous premarket approval requiring randomized clinical trials. Critics argue that current regulatory standards may not offer sufficient protection against AI products that ultimately provide limited utility.
Economic and Access Barriers
While proponents tout AI's potential for cost savings, implementation costs remain substantial. Healthcare organizations must invest in data infrastructure, digital pathology systems, and the human expertise required to develop, implement, and maintain AI solutions. The cost of converting to digital pathology alone can be prohibitive for smaller community practices.
Access to AI technologies remains limited, particularly in low-income and rural settings. A 2025 Current Oncology Reports review noted that AI's current application risks exacerbating existing health disparities if access remains concentrated in well-resourced academic medical centers.
For patients, coverage and reimbursement policies remain inconsistent. While some AI tests like ArteraAI Prostate have achieved Medicare coverage, many others are available only through self-pay models or as part of research studies.
Clinical Validation Gaps
Despite impressive performance metrics in research settings, many AI tools lack prospective validation in real-world clinical practice. A 2024 meta-analysis of AI-based tools in prostate cancer found that while AI shows promise for screening and diagnosis, systematic reviews reveal insufficient evidence for widespread clinical deployment due to methodological flaws and evaluation biases.
The effectiveness of AI varies significantly depending on imaging systems, scanner manufacturers, and acquisition protocols. Key limitations include variability in training datasets, algorithms, and evaluation criteria. Many published studies lack external validation on independent datasets, raising questions about generalizability.
What Oncologists Think
Physician attitudes toward AI remain mixed. A September 2025 Medscape survey found that approximately one-third of oncologists say AI has improved how they diagnose or stage cancer, another one-third disagree, and the rest are undecided. This division reflects both genuine uncertainty about AI's clinical impact and concerns about workflow integration, liability, and the "black box" nature of some algorithms.
A review of 19 studies involving more than 2,100 cancer patients found that most support AI only when it operates under physician supervision. Top patient concerns include depersonalization of care, privacy issues, and algorithmic bias.
The Path Forward: Realistic Expectations
AI represents a genuinely transformative technology for cancer care, but transformation will be evolutionary rather than revolutionary. The most successful implementations will:
-
Augment Rather Than Replace: AI works best as a "second set of eyes" or decision support tool rather than autonomous diagnostic system.
-
Focus on Specific Applications: Targeted applications (like detecting suspicious lesions on imaging or predicting specific treatment responses) are more achievable than comprehensive "continuous monitoring" systems.
-
Prioritize Transparency: Explainable AI that shows its reasoning builds trust with clinicians and patients.
-
Address Equity Proactively: Intentional efforts to include diverse populations in training datasets and validate performance across demographic groups are essential.
-
Establish Clear Value Propositions: AI implementations must demonstrate clear clinical benefits and cost-effectiveness, not just technical feasibility.
For prostate cancer patients specifically, AI-powered tools for risk stratification, biopsy analysis, MRI interpretation, and treatment selection are becoming increasingly available and may genuinely improve care quality. However, these tools work best when integrated into comprehensive care by experienced clinicians who understand both their capabilities and limitations.
Recommendations for Patients
-
Ask About AI Tools: When discussing diagnostic tests or treatment decisions, ask your physician if AI-assisted analysis is available and whether it might benefit your specific situation.
-
Understand Coverage: For tools like the ArteraAI Prostate Test, verify insurance coverage. Medicare Part B covers this test with zero out-of-pocket cost, but coverage varies for other insurers.
-
Recognize Limitations: AI tools provide additional information but don't replace the need for experienced clinical judgment. Your oncologist should explain how AI results factor into overall treatment recommendations.
-
Advocate for Equity: If you're part of an underrepresented group, ask whether AI tools used in your care have been validated in diverse populations.
-
Stay Informed: AI in cancer care is evolving rapidly. Reliable information sources include major cancer centers, professional societies like the American Society of Clinical Oncology, and patient advocacy organizations.
Conclusion
The submitted article's vision of AI-transformed cancer care with comprehensive continuous monitoring, early complication prediction, and universally personalized treatment represents an achievable future goal rather than current reality. While AI has made genuine, validated progress in specific applications—particularly imaging analysis, pathology review, and treatment selection—the technology faces significant challenges including algorithmic bias, data quality issues, regulatory gaps, and access disparities.
For prostate cancer patients, AI-powered tools are becoming increasingly available and may offer real benefits in risk assessment, treatment planning, and diagnostic accuracy. However, these tools are best viewed as sophisticated decision support systems that augment physician expertise rather than revolutionary autonomous systems that transform the entire care delivery model.
The promise is real, but so are the challenges. Responsible implementation requires ongoing vigilance about equity, rigorous validation, transparent deployment, and realistic expectations. The oncology community, healthcare systems, regulators, and patients must work together to ensure AI delivers on its genuine potential while avoiding overpromising and underdelivering.
Verified Sources with Formal Citations and URLs
FDA Regulatory and Device Information
-
U.S. Food and Drug Administration. "Artificial Intelligence and Machine Learning (AI/ML)-Enabled Medical Devices." Updated regularly. Available at: https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-aiml-enabled-medical-devices
-
Artera. "Artera Receives U.S. FDA De Novo Marketing Authorization for AI-Digital Pathology Software Revolutionizing Prostate Cancer Care." News release. August 13, 2025. Available at: https://www.businesswire.com/news/home/20250813857439/en/
-
U.S. Food and Drug Administration. "Artificial Intelligence for Drug Development." Updated February 20, 2025. Available at: https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development
-
Breast Cancer Research Foundation. "Clairity Breast FDA Approved." June 2, 2025. Available at: https://www.bcrf.org/blog/clairity-breast-ai-artificial-intelligence-mammogram-approved/
Clinical Research and Validation Studies
-
Lauritzen AD, Lillholm M, Lynge E, et al. "Early indicators of the impact of using AI in mammography screening for breast cancer." Radiology. 2024;311:e232479. DOI: 10.1148/radiol.232479
-
Twilt JJ, Saha A, Bosma JS, et al. "AI-assisted vs unassisted identification of prostate cancer in magnetic resonance images." JAMA Network Open. 2025;8:e2515672. DOI: 10.1001/jamanetworkopen.2025.15672
-
Esteva A, Feng J, van der Wal D, et al. "Prostate cancer therapy personalization via multi-modal deep learning on randomized phase III clinical trials." NPJ Digital Medicine. 2022;5(1):71. DOI: 10.1038/s41746-022-00613-w
-
Xiang J, Wang X, Li R. "Unique Stanford Medicine-designed AI predicts cancer prognoses, responses to treatment." Stanford Medicine News. January 8, 2025. Available at: https://med.stanford.edu/news/all-news/2025/01/ai-cancer-prognosis.html
-
Widman AJ, Shah M, Frydendahl A, et al. "Ultrasensitive liquid biopsy tech spots cancer earlier than standard methods." Science Daily. April 30, 2025. Originally published in Nature, June 14, 2024. Available at: https://www.sciencedaily.com/releases/2024/06/240614141855.htm
Liquid Biopsy and Early Detection
-
Karimzadeh M, et al. "Orion AI model for analyzing circulating orphan non-coding RNAs." Reported in multiple 2024 publications. Referenced in: Molecular Cancer. 2025. DOI: 10.1186/s12943-025-02369-9
-
Al-Daffaie FM, Semreen MH, et al. "AI-assisted liquid biopsies show promise for early cancer detection." Clinica Chimica Acta. 2025. Available at: https://www.news-medical.net/news/20251202/AI-assisted-liquid-biopsies-show-promise-for-early-cancer-detection.aspx
-
Materios A, et al. "DELFI model to evaluate cfDNA fragmentation." Multiple 2024 publications. Summarized in: Cancers (Basel). 2025 Sep 29;17(19):3165. DOI: 10.3390/cancers17193165
-
Venetis K, Dipasquale A, Singhal S, et al. "Cancer in a drop: Advances in liquid biopsy in 2024." Critical Reviews in Oncology/Hematology. May 28, 2025. DOI: 10.1016/j.critrevonc.2025.104647. Available at: https://www.sciencedirect.com/science/article/pii/S1040842825001647
Prostate Cancer-Specific AI Applications
-
Arita Y, Roest C, Kwee TC, et al. "Advancements in artificial intelligence for prostate cancer: optimizing diagnosis, treatment, and prognostic assessment." Asian Journal of Urology. February 21, 2025. DOI: 10.1016/j.ajur.2024.12.001. Available at: https://www.sciencedirect.com/science/article/pii/S2214388225000074
-
Flach RN, van Dooijeweert C, Nguyen TQ, et al. "Prospective Clinical Implementation of Paige Prostate Detect Artificial Intelligence Assistance in the Detection of Prostate Cancer in Prostate Biopsies: CONFIDENT P Trial Implementation of Artificial Intelligence Assistance." JCO Clinical Cancer Informatics. 2025 Mar;9:e2400193. DOI: 10.1200/CCI.24.00193
-
Nair SS, Muhammad H, Jain P, et al. "A novel artificial intelligence-powered tool for precise risk stratification of prostate cancer progression in patients with clinical intermediate risk." European Urology. 2024;S0302-2838(24):02496-5. DOI: 10.1016/j.eururo.2024.07.013
-
Myriad Genetics. "Myriad Genetics partners with PATHOMIQ to add artificial intelligence technology platform to its oncology portfolio." News release. February 24, 2025. Available at: https://investor.myriad.com/
-
Rannikko AS. "Artificial intelligence for prostate cancer diagnostics." Nature Cancer. 2025;6:1613–1614. DOI: 10.1038/s43018-025-01034-w. Available at: https://www.nature.com/articles/s43018-025-01034-w
Comprehensive Reviews and Meta-Analyses
-
Abdul Rasool Hassan B, Mohammed AH, Hallit S, et al. "Exploring the role of artificial intelligence in chemotherapy development, cancer diagnosis, and treatment: present achievements and future outlook." Frontiers in Oncology. 2025;15:1475893. DOI: 10.3389/fonc.2025.1475893. Available at: https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1475893/full
-
Wang J, Wang T, Han R, et al. "Artificial intelligence in cancer pathology: Applications, challenges, and future directions." CytoJournal. 2025;22:45. DOI: 10.25259/Cytojournal_272_2024. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC12134795/
-
Kehl KL, Elmarakeby H, Nishino M, et al. "Artificial Intelligence (AI) in Oncology: Current Landscape, Challenges, and Future Directions." Cancer Discovery. 2024 May 1;14(5):711–726. DOI: 10.1158/2159-8290.CD-23-1199. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC11131133/
-
Shaw ML, Drake J. "Five Ways AI Is Transforming Cancer Care—and Companies That Are Making It Happen." AJMC (The American Journal of Managed Care). December 2025. Available at: https://www.ajmc.com/view/five-ways-ai-is-transforming-cancer-care-and-companies-that-are-making-it-happen
-
"The Transformative Impact of Artificial Intelligence on Cancer Care Delivery." ACCC Buzz Blog. December 2, 2024. Available at: https://www.accc-cancer.org/acccbuzz/blog-post-template/accc-buzz/2024/12/02/the-transformative-impact-of-artificial-intelligence-on-cancer-care-delivery
Bias, Equity, and Ethical Considerations
-
Garcia-Saiso S, Marti M, Pesce K, et al. "Artificial Intelligence as a Potential Catalyst to a More Equitable Cancer Care." JMIR Cancer. 2024;10:e57276. DOI: 10.2196/57276. Available at: https://cancer.jmir.org/2024/1/e57276
-
Kader S, Kumar D, Bhimji SS. "Artificial Intelligence in Cancer Care: Addressing Challenges and Health Equity." Cancer Network. April 28, 2025. Available at: https://www.cancernetwork.com/view/artificial-intelligence-in-cancer-care-addressing-challenges-and-health-equity
-
"Is Artificial Intelligence Echoing Human Bias in Cancer Care?" Binaytara Foundation Cancer News. March 19, 2025. Available at: https://binaytara.org/cancernews/article/is-artificial-intelligence-echoing-human-bias-in-cancer-care
-
Gichoya JW, Thomas K, Celi LA, et al. "Artificial Intelligence and Machine Learning Technologies in Cancer Care: Addressing Disparities, Bias, and Data Diversity." Cancer Discovery. 2022;12(6):1423-1427. DOI: 10.1158/2159-8290.CD-22-0373. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9662931/
-
Singh A, Verma S, Kumar P. "Beyond the hype: Navigating bias in AI-driven cancer detection." Journal of Medical Systems. 2024. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC11546210/
-
Gichoya JW, Banerjee I, Bhimireddy AR, et al. "The Impact of Artificial Intelligence on Health Equity in Oncology: Scoping Review." JMIR Cancer. 2022;8(4):e39645. DOI: 10.2196/39645. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9667381/
-
Mohamed S, Khan S, Smith R. "Artificial Intelligence and Cancer Health Equity: Bridging the Divide or Widening the Gap." Current Oncology Reports. 2025;27:27. DOI: 10.1007/s11912-024-01627-1. Available at: https://link.springer.com/article/10.1007/s11912-024-01627-1
Regulatory and Safety Assessment
-
Cruz Rivera S, Aiyegbusi OL, Ives J, et al. "Benefit-Risk Reporting for FDA-Cleared Artificial Intelligence−Enabled Medical Devices." JAMA Network Open. 2024;7(10):e2441279. DOI: 10.1001/jamanetworkopen.2024.41279. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC12475944/
-
Petrick N, Sahiner B, Chen W, et al. "Artificial Intelligence in Breast Cancer Screening: Evaluation of FDA Device Regulation and Future Recommendations." Radiology. 2023;307(4):e222919. DOI: 10.1148/radiol.222919. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC10623674/
-
"AI Medical Devices: 2025 Status, Regulation & Challenges." IntuitionLabs. December 14, 2025. Available at: https://intuitionlabs.ai/articles/ai-medical-devices-regulation-2025
Digital Health and Technology Integration
-
Zhang Y, Wu X, Chen Z, et al. "Digital sensing technologies in cancer care: A new era in early detection and personalized diagnosis." Biomedical Signal Processing and Control. June 25, 2025;102:107180. DOI: 10.1016/j.bspc.2025.107180. Available at: https://www.sciencedirect.com/science/article/pii/S2590137025000780
-
García-Barberán V, Gómez Del Pulgar ME, Guamán HM, et al. "The times they are AI-changing: AI-powered advances in the application of extracellular vesicles to liquid biopsy in breast cancer." Extracellular Vesicles and Circulating Nucleic Acids. 2025 Feb 28;6(1):128–140. DOI: 10.20517/evcna.2024.51. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC11977355/
Patient and Provider Perspectives
-
Medscape. "Oncologists Divided on AI's Value in Diagnosing Cancers." September 19, 2025. Available at: https://www.medscape.com/viewarticle/oncologists-divided-ais-value-diagnosing-cancers-2025a1000oxq
-
Hilbers D, Nekain N, Bates A, Nunez JJ. "Patient attitudes toward artificial intelligence in cancer care: scoping review." JMIR Cancer. 2025;11:e74010. DOI: 10.2196/74010
-
Yang DD. "Artificial intelligence in prostate cancer." Harvard Health Publishing, Harvard Men's Health Watch. August 1, 2024. Available at: https://www.health.harvard.edu/mens-health/artificial-intelligence-in-prostate-cancer
Professional Organization Resources
-
National Cancer Institute. "NCI clinical trials get boost from public private partnership." News release. April 22, 2025. Available at: https://www.cancer.gov/about-nci/organization/cbiit/news-events/news/2025/nci-clinical-trials-get-boost-public-private-partnership
-
Cancer Research Institute. "AI and Cancer: The Emerging Revolution." July 12, 2025. Available at: https://www.cancerresearch.org/blog/ai-cancer
Prepared for the Informed Prostate Cancer Support Group Newsletter
December 2025
All sources verified and accessed December 18, 2025

Comments
Post a Comment